Science For Everyone: How Antimicrobial Resistance Impacts Agriculture, And What Must Be Done
[ad_1]
Antimicrobial resistance and agriculture: Welcome back to “Science For Everyone”, ABP Live’s weekly science column. Last week we discussed how genetic factors and biomarkers can be associated with preterm birth, and how such births can be prevented through genetic research. This week, we explain the impact of antimicrobial resistance on livestock and plant agriculture, how this affects humans, and what must be done to combat the threat.
Antimicrobial resistance is a phenomenon in which certain antibiotics no longer function against pathogens such as bacteria, viruses, parasites or fungi because they have developed the ability to withstand and defeat the drugs made to destroy them. As a result, the pathogens are not killed and continue to grow. Antimicrobial resistance is responsible for at least 1.27 million deaths worldwide annually.
Due to antimicrobial resistance, several infections cannot be prevented or treated. Since the pathogens change over time and do not respond to medicines, it becomes more and more difficult to treat certain infections, and the risk of severe illness increases.
Check all the stories appearing in ABP Live’s weekly science column here.
Antimicrobial resistance in livestock
Antibiotic resistance not only impacts humans but also plants and animals. Antimicrobials such as antibiotics, antifungals, antiparasitics, and antivirals are used worldwide in animals to improve their health, enhance their growth rates, and increase their productivity. However, certain microorganisms in these livestock may develop resistance against the antimicrobials, as a result of which those resistant genes are transmitted from one species to another.
Therefore, it is important to ensure that animals are administered safe and effective antimicrobials because antibiotic resistance in animals hampers food security, and leads to reduced food production, higher food safety concerns, greater economic losses to farm households, and environmental contamination.
Awareness of antimicrobial resistance is growing, and hence, several countries have phased out the use of antimicrobials in animal production. Several livestock producers believe that the benefits of antimicrobials offset the negative impacts, but this is a misconception.
MUST READ | Antibiotic Use Linked With Increased Risk Of Heart Attack And Stroke In Women. Here’s Why
Also, it is challenging to find the level of antimicrobial use that optimises the performance on animal farms.
According to the Organization for Economic Cooperation and Development (OECD), the use of animal production in most European countries has decreased dramatically over the last decade due to the phase-out of antibiotics growth promotion in the European Union in 2006, and also the reduction in the use of antibiotics for disease prevention because of increasing awareness of the long-term adverse impacts of antimicrobial resistance.
But large, emerging countries such as Brazil and China still use antimicrobials in animal production in large amounts because of the impact of antimicrobials on animal growth and profit margins, and to decrease biosecurity measures. There is also a lack of access to alternative interventions for farmers in those regions.
MUST READ | Triple Drug Combinations, Stem Cell Therapy — Science Advances And Potential Treatments For COPD In Future
Antimicrobial resistance in fish
Not only are antimicrobials used in livestock production, but also in aquaculture. All of this results in agriculture-related antimicrobial resistance.
Since there is increasing demand for livestock and fish products, producers have increased antimicrobial use in intensive production systems. China, Brazil and India are the current hotspots of antimicrobial resistance based on livestock intensification patterns, and Indonesia, Peru, Myanmar, Nigeria, and Vietnam are the future hotspots.
China is a hotspot for antimicrobial resistance based on aquaculture trends, and Thailand, Bangladesh, Chile, Indonesia, Vietnam, and India are future hotspots. Fish production may become problematic in these regions in the future due to antimicrobial use.
Transmission of antimicrobial resistance from animals to humans
Antimicrobial resistance can be transmitted from livestock agriculture to humans and from humans to animals. These are called negative spillover effects.
Antimicrobial resistant variants of Salmonella and Campylobacter are the zoonotic pathogens that are of greatest risk to human health. These organisms can be transmitted from animals to humans through food.
Several livestock have been found harbour methicillin resistant Staphylococcus aureus, and when humans consume these animals, the antimicrobial resistant pathogens and resistant genes are transmitted.
MUST READ | Missing World War II Pilot Located After 8 Decades By Forensic Scientists
Antimicrobial resistant pathogens are typically found in animals, animal food products, and agro-food environments in developing countries. However, there is a lack of surveillance systems as a result of which no reliable data on the level of antimicrobial resistance in animals and their products exists.
It is a known fact that antimicrobial resistant pathogens in animals and their products result in antimicrobial resistant infections in humans, but there is no sufficient literature from developing countries to draw firm conclusions on the extent of the impact of antimicrobial resistance on humans to animals, according to a report published by the International Livestock Research Institute (ILRI).
MUST READ | Science For Everyone: How Genetic Factors And Biomarkers Can Be Linked With Preterm Birth
The Apocalypse pig
The first pig which reportedly harboured a Gram-negative organism resistant to an antibiotic called colistin is known as the ‘Apocalypse pig’. Colistin is a last resort antibiotic, a term used to describe antibiotics that still have activity against resistant pathogens and are therefore used as a last line of treatment when other antibiotics fail.
However, if an organism has developed resistance against a last resort antibiotic, no other treatment option is likely to work on it. Colistin was shelved in the 1970s due to its nephrotoxicity, and was not used clinically for approximately 30 years, as a result of which resistance against it was very rare. However, some mutations resulted in colistin resistance in Escherichia coli and Salmonella isolates, early research showed.
Colistin was not used clinically for a long time, but several countries continued using it in agriculture.
MUST READ | India Has Maximum Preterm Births Globally, Say Experts. Know Prevalence And Survival Rate
According to a March 2017 study published in the journal Essays in Biochemistry, colistin-resistant organisms have been isolated from humans with no prior exposure to colistin. This means there is a possibility that the mcr-1 gene, which has been found to confer colistin-resistance to certain E. coli strains from food animals in China, spread from animals to humans.
The mcr-1 gene has been detected in multiple countries making it difficult to pinpoint the origin of antimicrobial resistance.
From November 1, 2016, the use of colistin as a feed additive for animals was banned in China.
Why multidrug-resistant superbugs are a major problem
There have been several other outbreaks of infectious disease caused by multidrug-resistant organisms acquired through food sources.
A multistate outbreak of multidrug-resistant Salmonella heidelberg in the United States occurred in 2014. This was linked to the consumption of chicken meat from one supplier.
Antimicrobials are used in huge amounts in factory farmed chickens to prevent diseases, and to prevent outbreaks in the crowded and unhygienic conditions. In 2017, the global annual consumption of antimicrobials in factory farmed chickens was 148 milligrams of antibiotic per kilogram of animal produced. Due to such incidents, there were public calls for ‘antibiotic-free meat’.
Several animals are raised on antimicrobials harbour superbugs, which are microorganisms that have developed antimicrobial resistance.
These multidrug-resistant superbugs are the real issue, and not the residual antibiotics in the meat.
This is because animals harbouring superbugs could serve as reservoirs of resistant organisms which could eventually find their way to human consumers through the environment or through direct contact.
MUST READ | Classification Of Preterm Babies Based On Gestational Age, And Their Body Weights And Lengths
How some organisms become multidrug-resistant
It is widely believed that antimicrobials that are not currently in clinical use can be used as growth promoters in feed animals because resistance to these compounds would not lead to resistance to clinically used antimicrobials.
However, the argument is false because pathogens express drug efflux pumps, or mechanisms in which they can expel different classes of compounds, including the antimicrobials used as feed additives. When organisms express efflux pumps and expel antimicrobials, they are likely to become resistant against a multitude of antimicrobial compounds. Therefore, mostly ill animals should be treated with antimicrobials. The prophylactic use of antimicrobials and utilisation as growth-enhancers must be re-considered.
Due to the growing prevalence of antimicrobial resistance in agriculture, sustainable food production is jeopardised.
Antibiotic resistance in plants
Apart from E. coli and Salmonella species, over-intensification of livestock farming can cause Klebsiella species and Enterobacter species to become resistant to antibiotics. These antibiotic resistant organisms are spread along the food chain: to humans when the cattle are consumed as food, and to plants when the cattle excreta is added as manure to the soil.
“Agriculture plays a pivotal role in our society, providing food and natural resources for the emerging global population. However, the growing prevalence of antimicrobial resistance in agriculture poses a serious threat to public health and sustainable food production. Due to the over-intensification of livestock (cattle) farming, pathogenic Escherichia coli, Enterococcus spp., Salmonella spp., Klebsiella spp., and Enterobacter spp. are readily spread by food chains between humans and cattle; or from soil to plants. Manure mixed with animal dung is frequently added to agricultural soils to enrich the soil nutritional content. However, it can also be a significant source of microbes resistant to antibiotics,” Dr Rakhi Chaturvedi, Department of Biosciences & Bioengineering, Indian Institute of Technology Guwahati, told ABP Live.
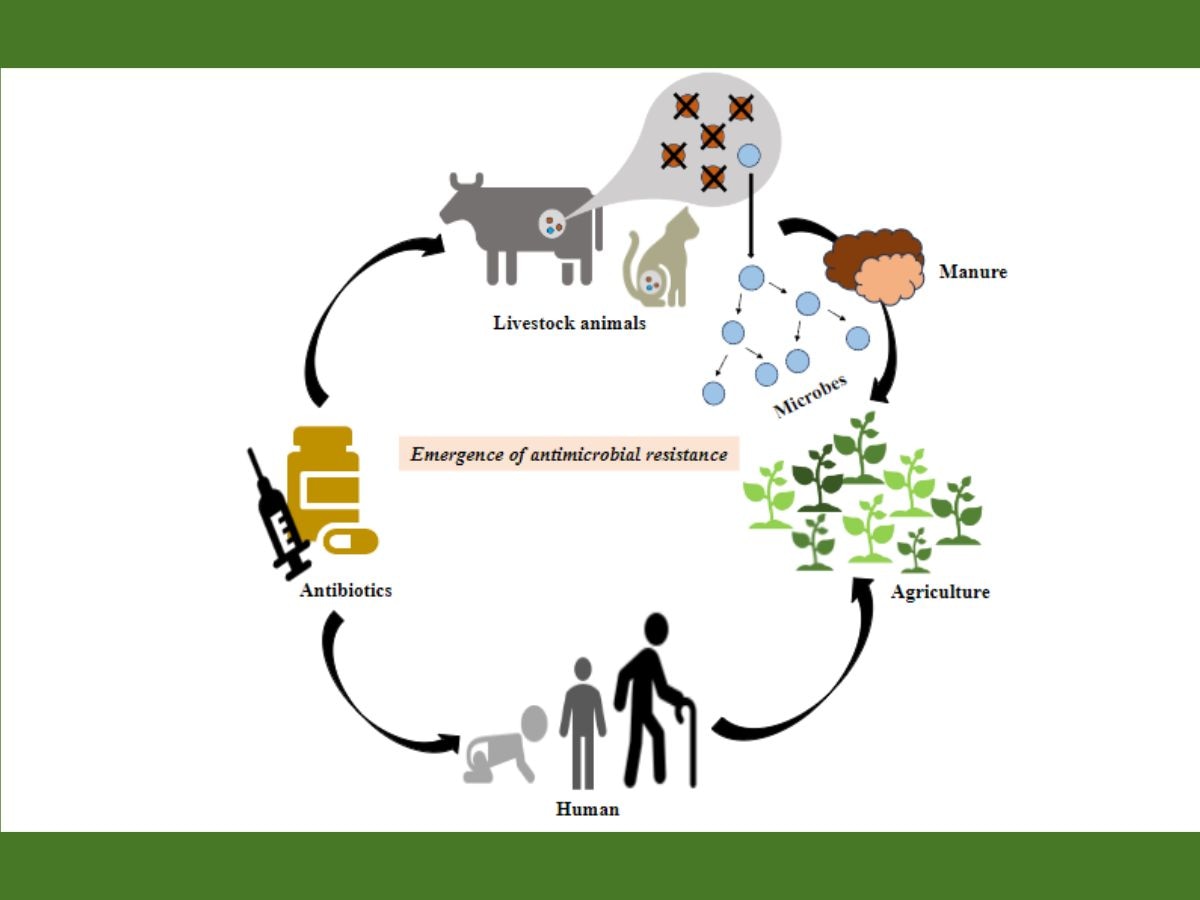
When plants are grown in soil contaminated with antimicrobial-resistant microbes or superbugs obtained from cow dung or animal excreta, the superbugs are transferred from the animals to the soil to the plants, and this can lead to the spread of multidrug-resistant infections in the agricultural field.
Not only are animals administered antimicrobials, but plants too are given antibiotics.
MUST READ | Can Diabetes Be Cured In The Future? Know Science Advances That May Make It Possible
These antibiotics include ampicillin, streptomycin, gentamicin, tetracycline, and oxytetracycline, among others. When high concentrations of these antibiotics are used in plants, the plant pathogens become resistant to the antibiotics.
“Transfer of antimicrobial-resistant bacteria from animals to plants through contaminated soil can contribute to the spread of multidrug-resistant infections in agricultural fields. Plant pathogens that are exposed to high concentrations of ampicillin, streptomycin, tetracycline, and other antimicrobials tend to become more resistant to them,” said Dr Chaturvedi.
How water bodies are a major source of antimicrobial resistant organisms
Scientists have isolated antibiotic resistant bacteria such as E. coli from water samples collected from ponds and lakes. Some major reasons behind the growth of multidrug resistant organisms in the ecosystem include indiscriminate use of antibiotics in animals for infections that are not too serious, inadequate treatment of biological waste, and dumping of animal waste into water bodies, which can reach humans.
This also leads to antibiotic resistance in fish, creating a burden on the aquaculture industry. When humans consume such fish, they obtain the antibiotic resistant genes. In this way, a vicious cycle continues.
“Water samples taken across various water bodies like ponds and lakes have shown varying degrees of antibiotic resistance in the bacteria isolated. One such example is E.coli. Indiscriminate use of higher antibiotics for innocuous infections, inadequate treatment of biological and other waste, and dumping animal waste into water bodies which are used for human consumption may be the reasons behind the growth of multidrug-resistant organisms in the ecosystem,” Dr Dilip Gude, Senior Consultant Physician, Yashoda Hospitals, Hyderabad, told ABP Live.
Water is a major source of antimicrobial resistant organisms because animal waste is dumped into water bodies, and as a result, antimicrobial resistant organisms also enter the water bodies. Cattle are often given antimicrobials without consultation with a veterinarian. This may cause them to develop antimicrobial resistance.
Several people consume cattle as food, causing antimicrobial resistance to enter the human food chain. Even wild animals are impacted because they often prey on cattle.
“Primarily, antimicrobial resistance can come through water. The reason it contains antimicrobials is because these drugs are directly given to the cattle. The antimicrobials enter the soil through cow dung, which is used as slurry or manure. Farmers often receive medicines for their cattle without a veterinarian’s evaluation. Even some veterinarians tend to prescribe excessive antibiotics. Many of these antimicrobials are also part of the animal food chain. This is how it enters the human food chain. Simultaneously, some of these cattle become prey to wild animals. This perpetuates the cycle through the food chain, water, and soil, ultimately reaching the human system,” Dr Meenakshi Venkataraman, Ecologist and International Director of the Projects Division of the Environmental Sustainability Rotary Action Group (ESRAG), told ABP Live.
MUST READ | How Increased Screen Time And Bad Postures Harm Neck And Spine, And What Must Be Done To Prevent Tech Neck
What must be done to control the spread of antimicrobial resistance among plants and livestock?
Effective implementation of national action plans is necessary to curb the risks posed by antimicrobial resistance. Such plans have been implemented for livestock agriculture in countries such as Brazil, the People’s Republic of China, and the Russian Federation.
There is a need for greater coordination among stakeholders to implement workable solutions, according to OECD. It is important to develop integrated surveillance and monitoring systems, improve regulations on the availability of antibiotics, and improve on-farm biosecurity practices, the OECD has suggested.
Enhanced public awareness, education, and training, and exploring alternative interventions and innovations to antimicrobials in animal health can help combat antimicrobial resistance.
MUST READ | What Was Thalidomide Tragedy? Over 6 Decades On, Australia Sorry For Babies Born With Birth Defects
Implementation of proper infection prevention and control measures, and improving overall health and welfare can address the issue of antimicrobial resistance. Some alternatives to antibiotics include vaccines and probiotics.
“To address the issue of antimicrobial resistance, it is important to promote responsible use of antibiotics for cattle, including implementing proper infection prevention and control measures, promoting alternatives to antibiotics, such as vaccines and probiotics, and improving overall health and welfare,” said Dr Chaturvedi.
Training and education alone can be relatively ineffective. However, if these are combined with strategies such as giving incentives on not using antibiotics, and making livestock producers and farmers accountable to the environment, better outcomes can be obtained.
MUST READ | Stroke Is Fourth Leading Cause Of Death In India, Global Cases Projected To Increase By 50 Per Cent By 2050
Several animal husbandry options can allow production without non-therapeutic antimicrobials, but developing countries have not widely adopted these practices.
Since there is a lack of evidence on antibiotic use in animals in developing countries, efforts should be made to increase research and fill the knowledge gaps.
According to the ILRI report, successes and failures of interventions to fight antimicrobial resistance should be rigorously evaluated to understand outcomes.
MUST READ | The Science Of Health: How Climate Change And Air Pollution Impact Heart Health, And What Must Be Done
Veterinarians should also be scrutinised to ensure that strong antibiotics are not prescribed to animals. It is important to ascertain the behaviours of farmers and veterinarians surrounding antimicrobial use to address imprudent antimicrobial use and create behaviour change within the agri-food sector, according to a November 2021 study published in the journal JAC Antimicrobial Resistance.
The barriers experienced by key stakeholders can be overcome by keeping in mind an evidence-based approach, and by incorporating behaviour change theory while designing strategies to prevent imprudent antimicrobial use.
The World Health Organization (WHO) released their ‘Global action plan’ on antimicrobial resistance in 2015, one of the objectives of which was to optimise the use of antimicrobial medicines in human and animal health by curbing the inappropriate or unregulated use of antimicrobial agents in agriculture, among other things.
MUST READ | Science For Everyone: Why Delhi Air Pollution Is So Severe, And What Needs To Be Done
The Australian government adopted a One Health approach in June 2015. One of the objectives of the approach is ‘Surveillance of antimicrobial resistance and antimicrobial usage in human health and animal care’.
By raising awareness, and through surveillance and careful monitoring, the Food and Agriculture Organization (FAO) helps prevent the development of antimicrobial resistance. It supports national action plans involving all stakeholders.
According to the study published in Essays in Biochemistry, monitoring programmes should be extended beyond antibiotics to biocides, which are substances used to destroy living things. Pesticides, fungicides, and herbicides are biocides.
MUST READ | Delhi Air Pollution: How Outdoor And Indoor Air Pollution Affect Male And Female Reproductive Health
When people suffering from viral infections consume high concentrations of antivirals without consulting a medical professional, the virus affecting them tends to become resistant to the medicine. Also, the consumption of antibiotics during viral infections can significantly contribute to antibiotic resistance.
The fact that untreated human waste can enter the soil and water bodies is a major cause for concern. Root vegetables grown in such contaminated soil may become antibiotic resistant due to the presence of antibiotic resistant bacteria in the soil. In fact, other microorganisms present in the soil can also become resistant to antibiotics due to interaction with other antibiotic-resistant bacteria.
“When it comes to viral infections, antivirals are appropriate, but often, people either avoid consulting a doctor or believe it’s the quickest remedy, leading to self-overdosing. Furthermore, it’s not just from animals; human waste, largely untreated, enters the system. Particularly concerning is the soil, especially in relation to root vegetables. It’s essential to realise that antimicrobials also impact organisms in the soil, where the highest concentration of microbial growth occurs. People tend to forget that soil is a living entity in itself,” said Dr Venkataraman.
Sustainable farming practices can play a key role in combating antimicrobial resistance, according to Dr Chaturvedi. “By adopting such measures, we can safeguard the future of agriculture and ensure food security while protecting both human and animal health.”
MUST READ | How Are Planets Made? NASA’s James Webb Space Telescope Makes Breakthrough Discovery
Check out below Health Tools-
Calculate Your Body Mass Index ( BMI )
[ad_2]
Source link